WHAT is BURNOUT?

WHAT is BURNOUT?
Burnout has emerged as a major problem plaguing 21st century among healthcare professionals. The term “burnout” was used by clinical psychologist Herbert Freudenberger in 1974. He used it to describe the consequences of severe stress and high ideals in “helping” professions. (-1)

He defined burnout as exhaustion resulting from “excessive demands on energy, strength, or resources” in the workplace, characterizing it by a set of symptoms including malaise, fatigue, frustration, cynicism, and inefficacy.
The concept of burnout among healthcare professionals is not new. Healthcare, as an industry, places numerous pressures on healthcare providers, including;

*The challenges of clinical work
*Work compression
*Time constraints
*Production pressure
*Competing demands
*Lack of control over one’s professional life
*Lack of control over work processes and scheduling
*Conflicting roles and relationships with leadership (-2)
*The stigma of psychological stresses and discourage physicians from seeking appropriate care.-5
*Rapid introduction of new technology and techniques.
*Demands of electronic health records

The electronic health record (EHR) is often blamed for increasing the burden of clinical documentation and decreasing the amount of time for personal conversation and connection with patients and families. (-5)
One study of medical interns reported that each intern spent less than eight minutes (less than five minutes in Turkey )with each patient per day . (-5)
Physicians are spending more time with documentation and clerical tasks and less time in dialogue with patients.(-5)

Only about 12% of total work time was spent in direct contact with patients, and 66% of the trainees’ time was spent in indirect patient care activities, such as placing and reviewing orders, communicating with other physicians, and writing and reading progress notes. (-5)
The Agency for Healthcare Research and Quality is estimating that burnout may affect 10–70% of nurses and, 30-50 % of physicians, nurse practitioners, and physician assistants. (-2)

Doctors and nurses, for example, who sacrifice themselves for others, would often end up being “burned out” – exhausted, listless, and unable to cope. (-1)
DeOliveira et al. found a risk of burnout in 41% of approximately 1,500 anesthesiology residents in a study. (-5)
Over the past two years, COVID-19 pandemic has greatly impacted physician wellbeing and mental health, with over 6 in 10 physicians (61%) reporting they experienced feelings of burnout. This is a significant increase from the 40% of reported physicians in 2018.
Burnout and depression have increased among physicians, while the rate of suicide has remained relatively the same.

Physicians Foundation released the results of a national survey in 2021, which finds that more than half (55%) of physicians ,who has considered, attempted or died by suicide in their career.
Researchers say ,beyond burnout, 39% of physicians report depression and about 400 physicians die by suicide each year, which is twice the rate of the general population. Considering that the average medical school has 126 students in each class, and so that’s an entire medical school equivalent of physicians per year.

The suicide rate among women doctors is about 130 percent higher than the general population, while men doctors experience a 40 percent higher rate. Nurses also report high rates of burnout and depression, as well as high rates of post-traumatic stress disorder symptoms. (-6)

Physicians have the remarkable distinction of more successful suicides than the general population. The risk of suicide and suicidal ideation increases in medical school but dramatically accelerates once trainees enter graduate medical education programs. (-5)
Most people pursue careers in medicine with a strong desire to help others, anticipate a fulfilling, satisfying career and life in return for the expense, effort, and delayed gratification associated with years of graduate medical education. (-5)

The desired or anticipated outcomes for smart, motivated, altruistic physicians do not include loss of productivity, lack of enjoyment of a hard-sought career, disengagement with patient care, compromised patient safety, and ultimately depression and even suicide. (-5)
What are the signs and symptoms of burnout?

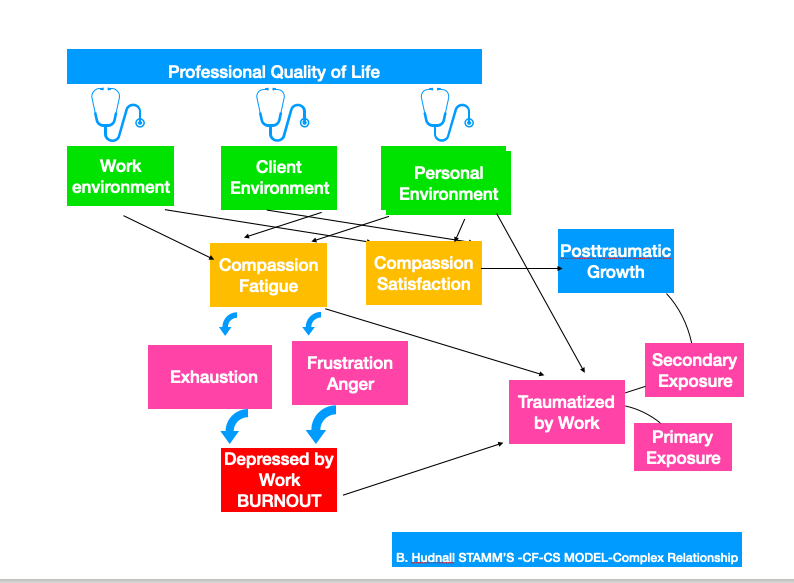
According to the social psychologist Christina Maslach; Burnout is consisting of three dimensions:
*Emotional exhaustion,
*Cynicism or depersonalization, alienation
*Low personal accomplishment ,efficiency, reduced performance (-2,5)
- Exhaustion: People affected feel drained and emotionally exhausted, unable to cope, tired and down, and don’t have enough energy.
- Alienation from (work-related) activities: People who have burnout find their jobs increasingly stressful and frustrating. They may start being cynical about their working conditions and their colleagues. At the same time, they may increasingly distance themselves emotionally, and start feeling numb about their work.
- Reduced performance: People with burnout are very negative about their tasks, find it hard to concentrate, are listless and lack creativity.(-1)
Which factors are linked to burnout?
- Biographical variables
- Sex affects the experience of burnout. In males, the most common signs of burnout are depersonalization followed by emotional exhaustion and cynicism. Females are more likely to experience emotional exhaustion as the first sign of burnout, later experiencing depersonalization and cynicism and a decreased sense of accomplishment. (-5)
- Individual factors: Personality traits can contribute to burnout:
- Perfectionistic tendencies.
- Exaggerated expectations.
- Pessimistic view of yourself and the world.
- High-achieving, Type A personality
- The culture of medicine. Medical students learn cultural imperatives such as service, excellence, competence, and compassion. These are important sources of pride for physicians, but each can become destructive if not balanced.The personal sacrifices required to provide service can result in feelings of deprivation or victimization if the self-sacrifice is extreme. (-5 ) Physicians routinely deny personal needs such as sleep and food in the course of their training and work
- System factors
- Characteristics of job and organization
How we can deal with BURNOUT ?
The concept of physician well-being is multidimensional.
Dealing with burnout requires the “Three R” approach:
*Recognize. Watch for the warning signs of burnout.
*Reverse. Undo the damage by seeking support and managing stress.
*Resilience. Build your resilience to stress by taking care of your physical and emotional health.

Institutional holistic wellness programs have implemented the programs to support their physicians and staff at times of severe stress, such as following an unexpected patient death. The term ‘‘Code Lavender’’ has been used to describe these activities, which mimic the terms ‘‘Code Red’’ and ‘‘Code Blue’’. Providers can call a Code Lavender, which brings support services to the providers who are experiencing severe stress. (-5)
The best approaches to enhancing physician well-being must address self-care as a professional imperative, and improving a balance between demands of altruism and self-care . (-5 )
- Cognitive behavioral therapy
- Exercise ,massage, yoga, meditation, spending time in nature
- Eating healthful foods and drinking plenty of fresh water
- Mindfulness training
- Institution, system-based strategies
- Enhancing physician professional development
- Screening tools for distress
- National considerations : Behavioral health conditions carry significant stigma compared with other medical conditions, even among healthcare providers.
- Living a creative, balanced life. Sing, dance, paint, sculpture, draw, write!

In this point we have a powerful pathway to help coping with burnout: Arts in Medicine.
Art enhances the health and links the body and mind together.Art offers the healthcare professionals an opportunity for creativity and self-expression that allows them to healthfully integrate their experiences and emotions instead of carrying them home or into the workplace.Creativity helps them contribute to their own decision making processes and recognize their feelings, thus giving them a branch to cling to life and an opportunity to express their feelings, thoughts, fears, and hopes. (AIM-7)
Through the creation ,they get a chance to focus their attention on something other than their pain and discomfort by being in the present . This opportunity gives physicians and healthcare professionals their self-control back.
Arts in Medicine transform and humanize the healthcare environment .
The Arts give medical professionals new tools for improving the diagnostic and communication skills .
For students in medical and other healthcare fields the arts can enhance their skills, and improve their observational diagnostic and empathic abilities.It helps them to understand patients in a different way and connect with them on a more humanizing level. (-AIM-7)
Art provides to rediscover the cooperation between creativity and medicine.The Art’s power of soothing, reflective and reparative provides to relief for the physicians and healthcare professionals who work in stress.(7,AIM )
Physicians should be advocates for the arts in general and more specifically in medical education and practice.(7AIM ,28)

The healthcare environment also plays an important role in improving the health and safety for staff, increasing effectiveness in providing care ,reducing errors ,and enhancing job satisfaction (7,AIM)

The supportive and functional environments in healthcare facilities from architectural design to art on the walls, from access to natural lighting to the healing gardens has a significant impact on reducing physicians, healthcare workers and patients stress ,improving health outcomes, enhancing patient safety and overall quality of care and reducing costs.(7,AIM)
The Arts in Medicine Research has focus on architecture or design issues .Studies confirmed that visual exposure to natural environments is effective in reduction of anxiety and stress (6,25).

Hospital gardens provide restorative and calming nature views and also can reduce stress and improve outcomes through other mechanisms ,for instance ,fostering access to social support and providing opportunities for positive escape and sense of control with respect to the stressful clinical settings.(6,26Tieman 2001).

One of the most significant benefits of hospital healing gardens is their effect on mood.( 6,27). They found that 95% of the garden users reported a change in mood:nearly 80% reported feeling more relaxed calmer ;25 % felt refreshed ,stronger ;22% said they were better able to think ,cope; 19% reported feeling better ,more positive; and 6% felt a religious or spiritual connection.

Spending time in nature(18) can influence markers of immune function; that Zumba dance classes can reduce blood pressure and triglyceride levels (19); and that community design, including walkability, can enhance glucose control. (20) The Recharge rooms within a hospital that provide an immersive sensory experience of nature, measurably reduced the physiological, hormonal, and behavioral consequences of stress experienced by frontline healthcare workers during the COVID-19 pandemic (6,21)

According to Creativity and Aging Study (2006) arts built sense of control for all age groups. Studies revealed an increase in the level of T cells which ward off bacterial infections and Natural Killer (NK) cells which combat cancer cells which reflects the influence of the mind on neurological centers of the brain and, in turn, on the immune system (6,9)

Mozart’s piano sonatas were analyzed for composite elements of relaxation by Conrad et al .(6,16) They found that Mozart music application; significantly reduce the amount of sedative drugs ,increase plasma concentrations of growth hormone ,decrease concentrations of interleukin six and epinephrine and lower blood pressure and heart rate.

Based on the effects of Mozart’s piano sonatas, the researchers propose a neurohumoral pathway by which music might exert its sedative action. Their model includes an interaction of the hypothalamic-pituitary axis with adrenal medulla via mediators of the unspecific immune system. (-7AIM.)
The biological influence of music enhances wellbeing, modulates the cardiovascular system, boost the immune system (6,22).
When we make art or music or dance together, we are literally “in it”together body, mind and spirit (7AIM )

The complex network of interconnected biological systems impacted by the arts and aesthetic experiences goes beyond the brain to encompass endocrine, immune, circulatory, and respiratory functions as well. We see, for example, that music played at a certain frequency decreases levels of cortisol, a hormonal marker of stress, while increasing oxytocin, a hormone sometimes used therapeutically to treat depression and anxiety (6,17).
A study in Neuroscience and Biobehavioral Reviews found that dance can increase the volume of the hippocampus, a brain structure that plays a role in forming new memories (6,11)

Painting, drawing, and other visual arts enable individuals dealing with PTSD to express themselves. One systematic review found that art therapy reduced common responses to trauma, such as anxiety, and depression .(6,23)
Poetry helps both patients and health professionals deal with end-of-life challenges (6,24)
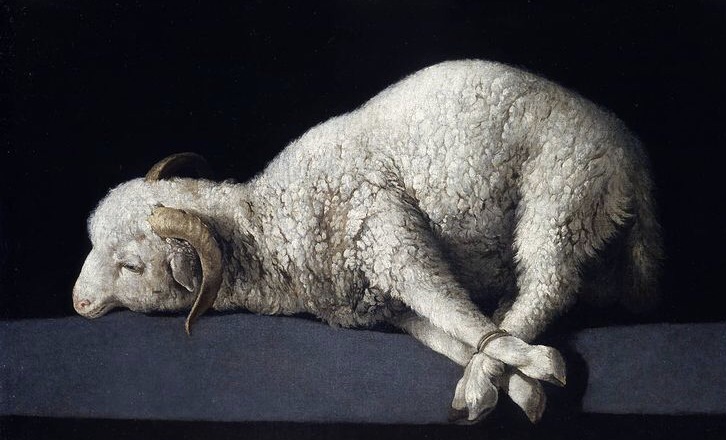
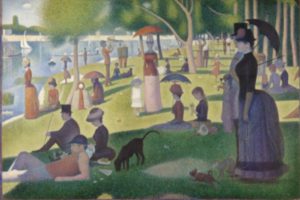
Paintings in sequence;1-George Frederic Watts /Hope 2-Rembrandt/ Anatomy Lesson of Dr. Deijman Rembrandt 3-Enrique Simonet/Autopsia 4-Zurbaran/Agnus Dei 5-Pere Borrell del Caso /Escaping Criticism 6-Edward Munch /The Sick Child 7-Jacques-Louis David /The Death of Marat 8-Alma Tadema/The Roses of Heliogabalus 9-James Jacques Joseph Tissot 10-Georges Seurat/Sunday Afternoon on the Island of La Grande Jatte 11-Claude Monet/The truth of Nature12-Jean-Honoré Fragonard /The Swing 13-Albert Aublet /Reading on the Garden Path 14-Johannes Vermeer/Girl with a Pearl Earring 15-Rosso Fiorentino /Angelo Musicante 16-Pablo Picasso/El Piano 17- Henri Matisse/Dance 18- Joseph Lefebvre/Woman playing a lute 19- Pierre Carrier- Belleuse /The Ballet Lesson
SOURCES. -*1-Depression: What is burnout? – InformedHealth.org – NCBI IQWiG health information -*2- Review Am J Health Syst Pharm /2018 Feb 1;75 (3):147-152. doi: 10.2146/ajhp170460. Epub 2017 Nov 28. Burnout syndrome among healthcare professionals /Patrick J Bridgeman, Mary Barna Bridgeman, Joseph Barone -*3. Review Pol Merkur Lekarski/ 2010 Mar;28(165):242-3./[Professional burnout among psychiatrists]/Anna Kamrowska1, Czesław Kamrowski – *4 . ‘Slave labor and mastery’:A psychoanalytic study of professional burnout Stijn Vanheule. -*5 . Self-care as a professional imperative: physician burnout, depression, and suicide s12630. -*6 NeuroArts Blueprint (Advancing The Science Of Arts , Health , And Wellbeing Is A Partnership Between The Johns Hopkins International Arts+Mind Lab,The Center For Applied Neuroaesthetics (IAM Lab ) And The Aspen Institute’s Health ,Medicine &Society Program (HMS) -*7. AIM-University Of Florida Center Of Arts In Medicine – *8 -https://www.helpguide.org/articles/stress/burnout-prevention-and-recovery.htm -*9.Coe& Lubach(2003);Kiecolt-Glaser,MGuiere,Robles&Glaser,(2002);Lutgendorf&Costanzo 2003 -*11. Teixeira-Machado, Arida, & de Jesus Mari 2019 -*16- Conrad et al 2007-*17 . Akimoto, Hu, Yamaguchi, & Kabayashi 2018. -*18. (Kuo 2015) -*19 . Araneta & Tanori 2015 -*20 . Mena, Sepulveda, Ormazábal Rojas, Fuentes, & Palomo 2017 -*21 . Mount Sinai Abilities Research Center n.d. -*22 . Global Council on Brain Health 2020).Hutschemaekers -*24 .Davies 2018.NA.-*25- Ulrich et al 1991 -*26 . Ulrich,Zimring,Joseph,Quan,Choudhary,2004 -*27. Cooper and Barnes 1995 -2005 -*28 . Gary Christensen is Director of the mental health clinic at the University of Minnesota’s Bolton health service and president of the Society for the arts in healthcare